In an annual report by the American Cancer Society, an estimated 1.9 million cancer cases and 609,360 cancer deaths will occur in the United States in 2022(1).
These figures highlight the importance of cancer detection to help physicians diagnose and treat this disease properly.
Scanning procedures like magnetic resonance imaging (MRI) or computed tomography (CT) can assist doctors in determining cancer’s presence in the body and the disease’s stage. Such scans are helpful, especially for detecting rare types of cancer like mesothelioma, which has four stages.
How does MRI work, and how effective is it in finding cancer in patients? What’s the difference between MRI and CT scans regarding cancer detection?
This article explains what MRI is and how effective this device is when used to detect cancer in patients. The write-up also explores the differences between a CT and MRI scan in detecting cancer.
How MRI Is Used to Detect Cancer
MRI, also called magnetic resonance, MR, and nuclear magnetic resonance (NMR) imaging, can assist doctors in detecting cancer in the body(2).
For example, healthcare providers can perform MRI scanning with mammography to detect breast cancer, especially among individuals with dense breast tissue or who are likely at a high risk of developing breast cancer(3).
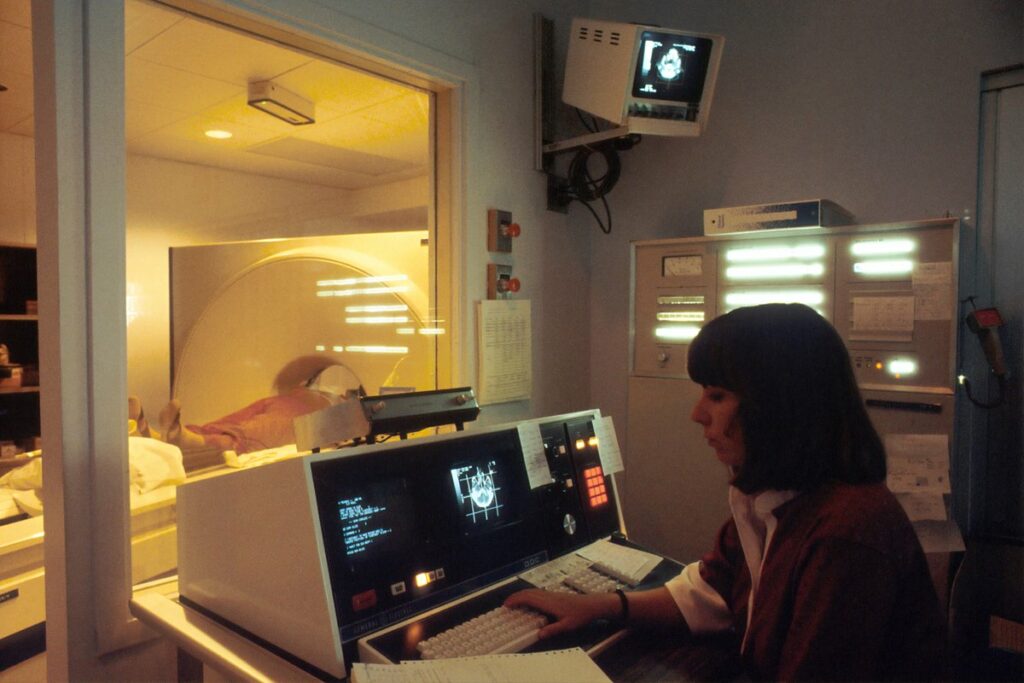
A radiologist or a radiology technologist are healthcare professionals who typically perform the MRI procedure on an individual.
A radiologist is a doctor who analyzes and interprets imaging tests to diagnose conditions(4). Meanwhile, a radiology technologist is a healthcare professional with special training and certification to perform an MRI scan.
An MRI scanner consists of a long tube or cylinder containing a large and powerful magnet. When undergoing an MRI, the patient lies on a table that can slide through the tube. Afterward, the machine’s strong magnetic field surrounds the individual.
The machine uses its magnetic force combined with a burst of radiofrequency waves to detect signals from the nuclei (centers) of hydrogen atoms inside the patient’s body. Afterward, a computer converts these signals digitally into a black-and-white image.
Healthcare providers typically use MRI to look into and evaluate the different structures inside a patient’s body, including(5):
- The brain and surrounding nerve tissue
- Chest and abdomen organs, such as the heart, liver, kidneys, biliary tract, spleen, pancreas, bowel, and adrenal glands
- Breast tissue
- The spine and spinal cord
- Pelvic organs, such as the bladder and reproductive organs
- Lymph nodes
- Blood vessels
MRI is generally safe and poses little risk to the average individual, provided they follow the appropriate safety guidelines(6).
This device is painless, so there is no need to perform any special procedures to prepare for this test(7). However, because MRI uses powerful magnets to produce images, the presence of metals can interfere with the scan.
Thus, if the individual has metallic objects like piercings or prostheses (artificial body parts) in their body, they must inform their doctor and technologist who is performing the scan.
The technologist can provide pillows or use straps to make the patient comfortable and help keep the individual from moving(8). The technologist places the part of the patient’s body being scanned in the center of the cylinder.
The scanned body part can feel a little warm during the exam(9). This sensation is normal, and the patient does not need to be worried.
When the MRI machine operates, the on-and-off switching of its magnets can make loud, clicking, whirring, or thumping noises. The technologist can provide the patient with earplugs or headphones with music to help block the noises during the scan.
MRI takes cross-sectional images of what is inside the body from different angles and provides views from the front, side, or above the scanned body part.
These images show the soft tissue body parts that can sometimes be difficult to see using other imaging methods(10). Because of this capacity, MRI can be an excellent way to find and pinpoint certain cancers.
Performing an MRI with contrast dyes is the best way to detect tumors, especially in the brain and spinal cord(11). By using MRI with contrast dyes, doctors can determine with improved clarity and accuracy whether or not a tumor is considered cancerous.
A contrast dye or contrast agent is a substance radiologists use to improve the clarity of an individual’s tissues and organs in medical images(12).
Physicians administer contrast dyes to a patient in one of three ways(13):
- Orally or through the mouth
- Rectally through the use of an enema
- Intravenously by injecting into a blood vessel
Although the contrast materials enter the individual’s body, these dyes do not permanently cause discoloration to the internal organs(14).
Instead, contrast dyes temporarily change how imaging tools interact with the body. Furthermore, the administered dyes do not produce radiation(15).
Some individuals may have a slight risk of an allergic reaction when using contrast material while undergoing an MRI(16). These reactions are often mild and controllable using medication.
On rare occasions, the contrast material can also cause the following side effects(17):
- Nausea
- Headache
- Pain at the site of the injection
If the patient experiences an allergic reaction, a healthcare provider should be available for immediate assistance.
In case the individual undergoing MRI is pregnant, healthcare providers generally do not perform MRIs using gadolinium contrast material. This enhanced procedure poses risks to the developing baby unless the exam is necessary(18).
Gadolinium can also cause complications for dialysis patients or those with severe kidney problems(19). Thus, healthcare providers rarely give this contrast material to these patients.
Radiologists can use MRI to look for indications that cancer may have spread or metastasized from where the tumor started to another part of the body.
Many laboratories performing MRI scans are located outside hospitals. Individuals can undergo such scans on an outpatient basis, meaning they do not need to be in a hospital for an MRI procedure(20).
These individuals are not required to follow a special diet or do anything to prepare for an MRI(21). However, they must follow any instructions given to them.
For example, if the patient has metal piercings, the individual must remove these items before getting an MRI scan.
Some individuals may have claustrophobia or a fear of enclosed spaces. Since an MRI machine is a small, enclosed tube, such patients may have issues undergoing a scan.
In this case, the physician can require the patient to take medicine to help the patient relax while inside the scanner. One medication is alprazolam (Xanax) to help manage claustrophobia and other anxiety-related conditions(22).
Other individuals who still have difficulties undergoing the procedure can consider talking with the technologist or patient counselor. In some cases, letting the patient view the MRI machine before the exam can help(23).
Patients needing more space around their bodies during the scan can opt for an open MRI.
Unlike a closed MRI, an open MRI has open space on two sides. An open MRI machine consists of two flat magnets placed over and under the patient. The ample space between these magnets is where the patient lies.
The open space can help alleviate an individual’s claustrophobia often associated with closed-bore MRI machines(24).
One study mentioned that MRI is not routinely used in clinical practice for patients with malignant pleural mesothelioma (mesothelioma of the lungs)(25).
However, the researchers also said that MRI might be better than CT for detecting invasion in the peritoneal (abdominal) and chest wall areas. MRI is often reserved for patients eligible for cancer surgery.
These findings suggest that MRI may be effective in detecting cancer, including rare ones like mesothelioma, and determining the stage of the disease.
After the technologist has produced the MRI images, doctors can use these images to recommend to the patient what cancer treatment to take, such as surgery, radiation therapy, or chemotherapy.
Difference Between MRI and CT Scan for Cancer Detection
Healthcare providers usually prefer MRI scans instead of CT scans when these providers need to look at the soft tissues or non-bony parts of an individual’s body(26). MRI scans are also relatively safer than CT scans because MRI does not use X-rays that can cause damaging ionizing radiation.
Compared to CT scans and X-rays, MRI scans can take much clearer pictures of an individual’s body parts, including the brain, spinal cord, muscles, nerves, tendons, and ligaments(27).
However, some patients have metal implants or devices that should not be exposed to the MRI’s powerful magnets. Individuals with such devices cannot undergo an MRI scan(28).
Individuals with any of the following implants should not enter the MRI scanning area unless a radiologist or technologist tells them to do so(29):
- An implanted pacemaker or defibrillator
- A cochlear (ear) implant
- Clips for brain aneurysm
- Metal coils placed inside blood vessels
In these cases, the doctor can recommend another scanning method, such as a CT scan.
While the MRI scanner is a tube-shaped structure, the CT scanner is a large, donut-shaped device with a short tunnel in the center. To undergo a CT scan, the patient must lie on a narrow table that slides through this tunnel.
Once the patient is inside the CT scanner, a ring-shaped gantry containing an X-ray tube and electronic X-ray detectors opposite each other starts rotating around the individual.
A technologist processes the imaging information in a computer workstation in a separate room. This place is where the technologist operates the CT scanner and monitors the patient’s examination.
The technologist also has direct visual contact with the patient and can talk to and hear the patient using a microphone and speaker.
Unlike an MRI that uses magnets to produce images, CT scans send radiation through the body to create a computerized, 360-degree view of the scanned body part.
A CT scan works similarly to other X-ray exams, wherein different body parts absorb X-rays in varying amounts(30). This difference in X-ray levels helps the radiologist distinguish one body part from another when viewing a CT image.
With CT scanning, several X-ray beams and electronic detectors rotate around the patient and measure the amount of radiation absorbed throughout the individual’s body(31).
The exam table where the patient lies can move during the procedure depending on what body part needs to be scanned.
A CT scan can produce multiple images. So technologists use a unique computer program to analyze and process the pictures to produce two-dimensional cross-sectional images of the patient’s body or body part. Afterward, the system shows the images on a computer monitor.
CT scans create images of soft tissues and bones. However, these scans are less effective than MRIs at revealing subtle differences between tissue types(32).
The technologist performing the CT scan can ask the patient to hold their breath during the scan. Any motion, such as breathing and other body movements, can produce blurred images, leading to a loss of image quality(33).
MRI scans can take 30 to 50 minutes, depending on the exam type and the equipment used(34). The patient’s healthcare provider can provide a more exact time range according to the specific reason for the procedure.
On the other hand, a CT scan appointment can last for approximately 15 minutes(35). However, if the procedure requires a contrast, such as one taken orally, the scan can take up to 1 hour and 15 minutes.
Similar to MRI scans, CT scans are generally painless(36). Still, some individuals can experience discomfort from not moving for several minutes. These individuals can find a CT exam stressful, especially if they have difficulty staying still or are nervous, anxious, or in pain.
In such cases, the nurse or technologist, under a doctor’s supervision, can offer medication to help the individual tolerate the CT exam.
Another significant difference is that MRI scanning is typically more expensive than CT or X-ray imaging(37).
A study in Ontario showed that MRI utilization in cancer patients accounted for approximately 10% of all MRI scans(38). On the other hand, CT scanning in cancer patients comprised 24% of all CT scans.
These results indicate that only a minority of MRI and CT scans are used for cancer detection. However, the study also mentioned that many cancer patients travel outside their region to undergo diagnostic imaging. Thus, these findings may help influence decisions about the location of new MRI and CT scanners.
Individuals interested in further learning about cancer detection can visit the American Cancer Society website or call 1-800-227-2345.
- Cancer Facts & Figures 2022
https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2022.html - MRI for Cancer
https://www.cancer.org/treatment/understanding-your-diagnosis/tests/mri-for-cancer.html - MRI (Magnetic Resonance Imaging)
https://my.clevelandclinic.org/health/diagnostics/4876-magnetic-resonance-imaging-mri - Ibid.
- Ibid.
- Ibid.
- MRI for Cancer
https://www.cancer.org/treatment/understanding-your-diagnosis/tests/mri-for-cancer.html - Ibid.
- Ibid.
- Ibid.
- Ibid.
- Having an Exam That Uses Contrast Dye? Here’s What You Need to Know
https://blog.radiology.virginia.edu/medical-contrast/ - Contrast Materials
https://www.radiologyinfo.org/en/info/safety-contrast - Ibid.
- Ibid.
- MRI (Magnetic Resonance Imaging)
https://my.clevelandclinic.org/health/diagnostics/4876-magnetic-resonance-imaging-mri - Ibid.
- Ibid.
- MRI for Cancer
https://www.cancer.org/treatment/understanding-your-diagnosis/tests/mri-for-cancer.html - Ibid.
- Ibid.
- Prevention of Claustrophobia Induced by MR Imaging: Use of Alprazolam
https://www.ajronline.org/doi/pdfplus/10.2214/ajr.156.3.1899765?src=recsys - MRI for Cancer
https://www.cancer.org/treatment/understanding-your-diagnosis/tests/mri-for-cancer.html - MRI (Magnetic Resonance Imaging)
https://my.clevelandclinic.org/health/diagnostics/4876-magnetic-resonance-imaging-mri - Imaging of malignant pleural mesothelioma: it is possible a screening or early diagnosis program?—a systematic review about the use of screening programs in a population of asbestos exposed workers
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5830569/ - MRI (Magnetic Resonance Imaging)
https://my.clevelandclinic.org/health/diagnostics/4876-magnetic-resonance-imaging-mri - Ibid
- CT Scan Versus MRI Versus X-Ray: What Type of Imaging Do I Need?
https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/ct-vs-mri-vs-xray - MRI for Cancer
https://www.cancer.org/treatment/understanding-your-diagnosis/tests/mri-for-cancer.html - Body CT
https://www.radiologyinfo.org/en/info/bodyct - Ibid.
- CT Scan Versus MRI Versus X-Ray: What Type of Imaging Do I Need?
https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/ct-vs-mri-vs-xray - Body CT
https://www.radiologyinfo.org/en/info/bodyct - MRI (Magnetic Resonance Imaging)
https://my.clevelandclinic.org/health/diagnostics/4876-magnetic-resonance-imaging-mri - Preparing for Your CT Scan
https://health.uconn.edu/radiology/wp-content/uploads/sites/195/2020/01/Radiology-CTscan.pdf - Body CT
https://www.radiologyinfo.org/en/info/bodyct - MRI (Magnetic Resonance Imaging)
https://my.clevelandclinic.org/health/diagnostics/4876-magnetic-resonance-imaging-mri - Evaluation of CT and MRI scanning among cancer patients in Ontario
https://pubmed.ncbi.nlm.nih.gov/21724124/